Is there a link between Alzheimer’s disease and infections?
by admin
The effect of vaccines on the progression of Alzheimer’s disease in the UK and Wales: A case study from a Canadian man in Columbia
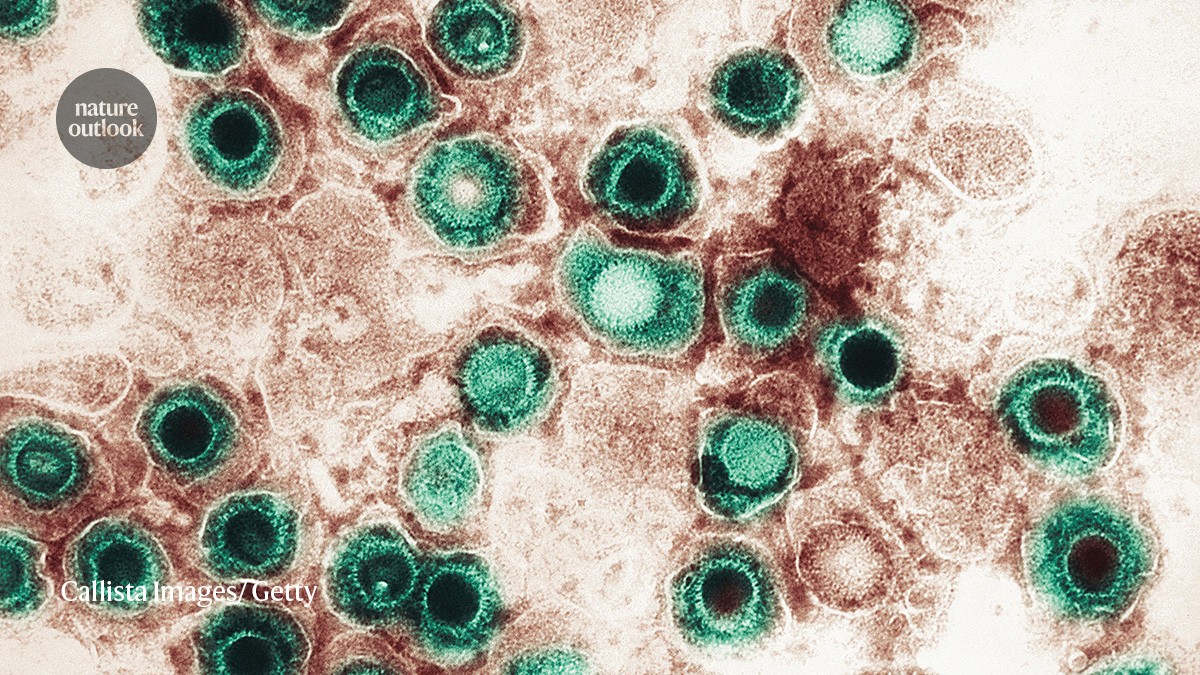
The possible involvement of VZV and otherviruses in people can cause damage to the immune system if reactivation occurs. But there is evidence tentatively linking numerous infectious agents to Alzheimer’s, and some researchers think that there could be a more generic mechanism at play — almost any pathogen that accesses the brain might shift Alzheimer’s into overdrive.
Scientists’ understanding of Alzheimer’s continues to grow, and could lead to new avenues for treatment and prevention. A woman from rural Columbia has a collection of rare genetic defects and inspiring one line of attack. And growing evidence suggests that pathogens might play a part in the development and progression of Alzheimer’s. Better care for all could be achieved by researchers getting to grips with mechanisms behind the differences in disease progression between the sexes. The work is under threat in the US with funding cuts ordered by President Donald Trump. Even the fight against Alzheimer’s disease is not safe from US politics.
Measuring antiviral antibodies circulating in the blood is also less than ideal, because they could be the result of viral reactivation anywhere in the body, not just the brain. And direct detection of viruses in brain-tissue samples is extremely difficult because it requires ultrasensitive molecular methods. “A lot of the push back against this research is coming from issues with the validity of the techniques for detecting viral particles in autopsy specimens,” says Garden.
Tanzi believes in the latter hypothesis. “Every time you have a vaccine, you amp up the peripheral immune system and monocytes get into the brain and help clear amyloid,” he says, referring to a subset of immune cells that help to fend off infectious agents and eliminate damaged cells.
This bias is overcome with Natural experiments based on how the shingles vaccine was rolled out in different nations. A study8 from his team has evaluated electronic health-care records in England and Wales, where there was a birth-date-based cut off for eligibility to receive the vaccine when it was rolled out. The difference in age at the time of start of the programme meant you had a huge difference in ever getting vaccinations. Otherwise, the demographics of these two cohorts were largely identical. The study showed a significant reduction in the risk of both diagnosis of dementia and death from dementia for women. The reduction in women was more than fivefold greater than that in men, in whom the observed protective effects were not statistically significant. Geldsetzer adds that the data indicate that there was a roughly 20% reduction in the odds of developing dementia in the seven-year follow-up period after receiving the shingles vaccination.
Since then, he and others have made a compelling case for the association of Alzheimer’s with a strong inflammatory response that suppresses neuronal function and accelerates the formation of amyloid-β plaques and tau tangles. “Inflammatory mediators are present in the cerebrospinal fluid as soon as amyloid starts to accumulate in the brain,” says Gwenn Garden, a neurologist at the University of North Carolina at Chapel Hill. lifestyle and environmental factors might contribute to inflammation in the brain which contributes to the development of Alzheimer’s, but is caused by a feedback loop that leads to plaque formation.
Shingles arises after the reactivation of the varicella zoster virus (VZV), which typically causes chickenpox early in life before becoming dormant for many decades. It is characterized by a painful rash that may be related to Alzheimer’s disease and other forms of dementia.
This condition, in which memory loss and confusion build over a long period of time, was once viewed as an unstoppable force or a natural consequence of aging. Today, we know that neither is true. Although Alzheimer’s is not yet curable, a handful of treatments can slow its progression, and much work is being done to try to further turn the tide.
The first disease-modifying therapies for Alzheimer’s target the peptide amyloid-β, which clumps together in the brain. Clearing these deposits slows cognitive decline. The task now is to achieve stronger effects by building on anti-amyloid therapy or combining it with drugs that target other aspects of the disease.
The development of blood tests to differentiate between Alzheimer’s and other forms of dementia is another major breakthrough over the past five years. Concerns over the misuse of these diagnostics are already present, even though they look to be crucial tools for physicians and researchers.
Comment on Percolation Effects in $epmp$ Decays of p-pbar Annihilations”
We would like to acknowledge that Eli Lilly & Company provided financial support in the production of this Outlook. Nature is solely responsible for all editorial content.
A study has shown that a vaccine reduces the chances of developing dementia by 20% in the seven-year follow-up period after receiving it. The study involved over 13,500 people in the UK and Wales who received one of three shingles vaccines between 2006 and 2010. In the study, those who received shingles vaccine had a 30% reduced risk of developing dementia than those who didn’t.