Child growth is faltering in low resource settings
by admin
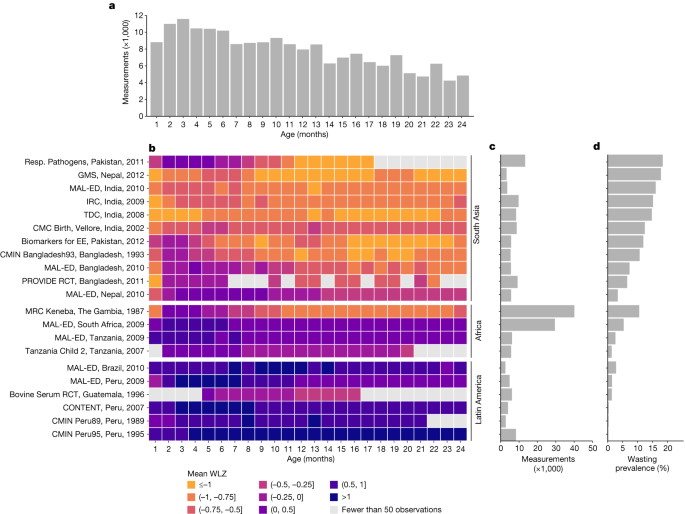
Using randomized and longitudinal studies of the ki project to quantify the incidence proportion of wasting between birth and 24 months of age in low-income countries
On April 1st, we included all of the randomized and longitudinal trials that were available through the ki project, which were done in LMICs and used children between birth and 24 months of age. We included all children under 24 months of age, assuming months were 30.4167 days, and we considered a child’s first measure recorded by 7 days after birth as their anthropometry at birth. Four additional studies with high-quality mortality information that measured children at least every 6 months were included in the mortality analyses (The Burkina Faso Zinc trial, The Vitamin-A trial in India, and the iLiNS-DOSE and iLiNS-DYAD-M trials in Malawi).
Incident proportion of wasting was calculated during a defined age range (for example, 6–12 months) as the proportion of children not wasted at the start of the period who became wasted during the age period (the proportion of children who had the onset of new episodes during the period). Period prevalence would include any children who had a measurement ofWLZ -2 in the period, as well as children who started the period wasted. The incidence proportion excludes the children who were wasted at the start of the period.
We stratified the above outcomes of interest within the following subgroups: child age (grouped into one-, three- or six-month intervals, depending on the outcome); region of the world (Asia, sub-Saharan Africa and Latin America); month of the year; and the combinations of the above categories. We also pooled wasting-incidence proportion by categories of three country-level characteristics: the percentage of gross domestic product devoted to healthcare goods and spending (obtained from the United Nations Development Programme; https://hdr.undp.org/); the percentage of the country living on less than US$1.90 per day; and under-5 mortality rates (both obtained from the World Bank; https://databank.worldbank.org/source/world-development-indicators). Within each country, in years without available data, we linearly interpolated values from the nearest years with available data and extrapolated values within five years of available data using linear regression models based on all available years of data.
We conducted a two-stage individual participant meta-analysis, estimating wasting outcomes within specific cohorts and pooling estimates within each age stratum using random-effects models. For example, we estimated each age-specific mean using a two-step process. The pooled age-specific means allowed for a random effect of the mean in each cohort. We estimated overall effects, and pooled estimates for specific South Asian, African or Latin American groups. We repeated the pooling of all statistics presented in the figures using fixed-effects models as a sensitivity analysis (Supplementary Note 2). There is a companion paper with more detail on the pooling methods. The pooling was done using a function in the metaphor package in the R language. Median durations were pooled across cohorts using the unweighted median of medians method60.
Seasonal patterns in the average rainfall over three consecutive three-month periods based on cubic splines from the Danish Department for Health and Statistics (DHS) program
Smoothes used in the figures were fitted using two methods. We estimated approximate simultaneous 95% CIs around the cubic splines using a parametric bootstrap that resampled from the posterior the generalized additive model parameter variance–covariance matrix62.
The season of peak rainfall was defined as the three-month period with the highest mean rainfall. Mean differences in WLZ between three-month quarters was estimated using linear regression models. We compared the consecutive three months of the maximum average rainfall over the study period, as well as the three months prior and three months after the maximum-rainfall period, to a reference level of the three months opposite the calendar year of the maximum-rainfall period. We used all WLZ measurements of children under two years of age (for example, if June–August was the period of maximum rainfall, the reference level is child mean WLZ during January–March).
Estimates were not adjusted for seasonal effects onWLZ because we assumed that they were non-exchangable. Mean differences in WLZ were pooled across cohorts using random-effects models, with cohorts grouped by the Walsh and Lawler seasonality index65. Cohorts from years with a seasonal index greater than or equal to 0.9 were classified as occurring in locations with high seasonality; cohorts with a seasonal index less than 0.9 and greater than or equal to 0.7 were classified as occurring in locations with medium seasonality; and cohorts with a seasonal index less than 0.7 were classified as occurring in locations with low seasonality.
We downloaded standard DHS individual recode files for each country from the DHS program website (https://dhsprogram.com/). From each country, we used the most recentDHS data for individual womens, household and length and weight, and we estimated the mean ages of LAZ, WAZ andWLZ from ages 0 to 24 months within each DHS survey. See a companion paper for further details on the DHS data cleaning and analysis19. We compared DHS estimates with mean LAZ, WAZ and WLZ by age in the Ki study cohorts with penalized cubic splines with bandwidths chosen using generalized cross-validation63. We did not seasonally adjust DHS measurements.
At birth, we consider the child at risk of incident outcomes if there are exposures before birth. We classified children who were wasted as stunting due to the fact that they were born stunted.
We compared outcomes across categories of exposures to estimate measures of association.
The comparison levels of exposure to LAZ at birth, 6 months, and 24 months are the mean difference. The z-scores used were the measures taken closest to the age of interest and within 1 month of the age of interest, except for z-scores at birth which only included a child’s first measure recorded by 7 days after birth. LAZ,WAZ and weight were calculated.
The cumulative incidence ratios for the incidence of outcomes in 6 months and 24 months are different than the ones for birth and 6 months.
Mean z-scores by continuous age, stratified by levels of exposures from birth to 24 months were fit within individual cohorts using cubic splines with the bandwidth chosen to minimize the median Akaike information criterion across cohorts61. Each exposure category has been estimated separately. We pooled spline curves across cohorts into a single prediction, offset by mean z-scores at one year, using random-effects models62.
The population intervention effect was the generalization of population risk and is defined as the change in population mean z-score if the whole population was exposed to the same risks. For each exposure we chose the category with the highest mean LAZ orWLZ based on prior literature.
For each exposure, we used the directed acyclic graph framework to identify potential confounders from the broader set of exposures used in the analysis65. We did not adjust for characteristics that were assumed to be intermediate on the causal path between any exposure and the outcome, because while controlling for mediators may help adjust for unmeasured confounders in some conditions, it can also lead to collider bias66,67. Detailed lists of adjustment covariates used for each analysis are available in Supplementary Note 1. There could be residual confound in cohort-specific estimates, since founders weren’t measured in every cohort.
Analyses used a complete-case approach that only included children with non-missing exposure and outcome measurements. For additional covariates in adjusted analyses, we used the following approach to impute missing covariate values68. If there were at least 50% missingness in a co-variable, all children were subjected to an indicator variable for missingness in the adjustment set. A potential adjustment set excluded covariates with over 50% missingness. Children were used as independent units instead of measurements when calculating the median to make sure children were not over-represented.
We did not estimate relative risks between a higher level of exposure and the reference group if there were 5 or fewer cases in either stratum. We still estimated the relative risks if the reference and other exposure Strata were not sparse. For rare outcomes, we only included one covariate for every 10 observations in the sparsest combination of the exposure and outcome, choosing covariates based on ranked deviance ratios.
Pooling of PAFs of exposure to cumulative incidence of wasting and stunting: A model for the outcome prevalence of survival with symmetric confidence intervals
$${\rm{PAF}}\,95 \% \,{\rm{confidence}}\,{\rm{interval}}=\frac{{\rm{PIE}}\,95 \% \,{\rm{confidence}}\,{\rm{interval}}}{{\rm{Outcome}}\,{\rm{prevalence}}}\times 100$$
For PAFs of exposure to the cumulative incidence of wasting and stunting, the pooledcumulative incidence was replaced for the outcome prevalence in the equations. We used this method instead of direct pooling of PAFs because unlike PAFs, PIEs are unbounded with symmetrical confidence intervals.
We have used randomized and longitudinal studies of ki project to quantify the incidence of the proportion of wasting between birth and 24 months of age in low-income countries. We estimated wasting outcomes within specific cohorts and pooling estimates within each age using random-effects models. The pooled age-specific means allowed for a random effect of the mean in each cohort.