Researchers are able to help to shepherd cancer vaccines
by admin
Hyper-personalised treatments for brain tumours: from gene-engineered cells to cancer vaccines, with applications to a 20-year-old woman
It is not the only people that could benefit from hyper-personalized therapies. Scientists and regulators must work together to ensure the benefits are spread.
When researchers first began to test engineered immune cells designed to fight cancer about 20 years ago, there was a scepticism. The scientific potential might be clear, but what about the economics of such a complex and specialized therapy? Each dose would have to be made afresh, with cells from an individual being shipped to a centralized laboratory, genetically engineered using sophisticated techniques and shipped back for reinfusion. The process would take too long and be expensive. Regulators wouldn’t be comfortable with the safety of such a process.
Both approaches are fraught with challenges. Many of them are not scientific, similar to the early days of CAR-T therapy. But by guiding regulators and developing flexible platforms for producing bespoke treatments, researchers can help to shepherd therapies to the people who need them.
Researchers have long chased after vaccines that could rally the immune system against tumours, similarly to how vaccines rouse defences against pathogens. Companies can now sequence portions of a person’s tumour and select those most likely to be visible to the immune system. The mRNA molecules corresponding to those regions are synthesized, then encapsulated in fatty particles and injected — much like mRNA COVID-19 vaccines. From start to finish, the process takes as little as a month.
An n-of-1 therapy is a term that highlights the statistical challenges of interpretation of results from a sample of one and how it can be difficult to design and sell a therapy with a single person market. But the name is potentially misleading and stigmatizing. A cancer vaccine based on an individual’s tumour could also be considered an n-of-1 therapy, yet this approach has attracted heavy investment from the pharmaceutical industry because the same process can be extended to many other people with cancer.
Ghosh and his collaborators were racing to design a one-off treatment that would edit the DNA in the 20-year-old woman’s brain cells and get them to stop producing toxic proteins. It was an approach that had never been tried before, with a long list of reasons for why it might not work.
Uditi’s family didn’t wait because the research pace was too slow. They needed a sprint, a team of researchers willing to take on not only the scientific challenge but also the emotional heft and high risk of failure that come with attempting something that had never been done. “What we were trying to do was really almost in the realms of science fiction,” Ghosh says.
There were a lot of unknowns in the base-editing project. In addition to stem cells in the lab, the team needs to conduct further experiments on which base-editing systems would work best, where and how to deliver components into the body, and if the process generated any unwanted changes to the DNA sequence. They would need to do experiments in mice to test the safety and efficacy of the treatment. The facility for producing base-editing components was approved by India’s regulators.
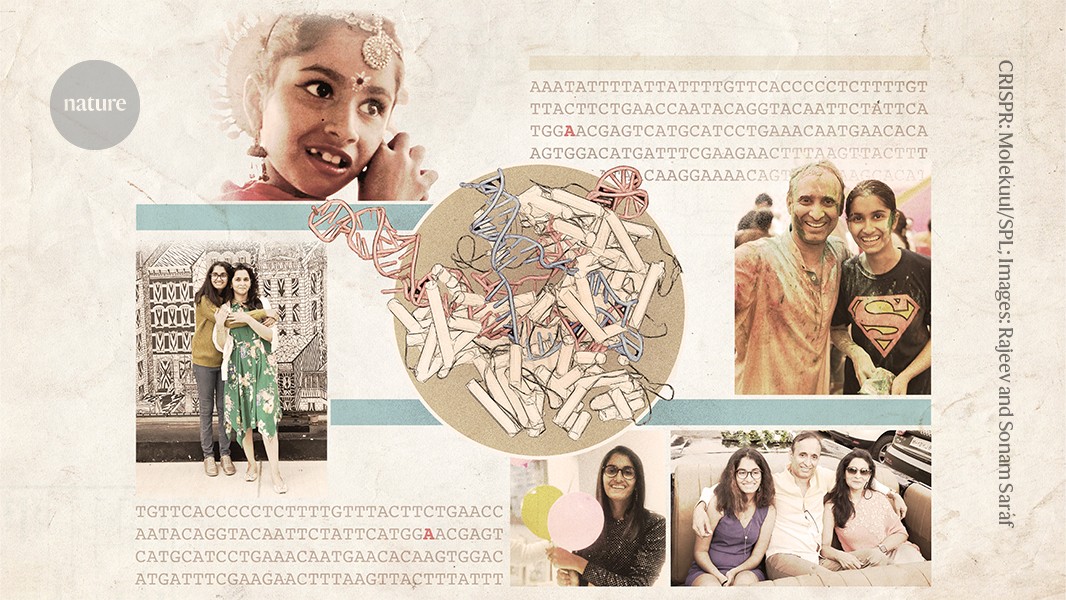
A moment of crisis for Uditi, a 10-year old girl who was always in a hurry to attend a birthday party or a festival
Uditi was always in a hurry as a young girl. Seizing any excuse to celebrate — whether it was a birthday or a festival — she would buzz around the house getting ready hours ahead of everyone else, peppering her mother with urgent requests. She greeted family and friends with cuddles and kisses and brightened parties with her laughter and dancing.
There was no indication of trouble for the first nine years. It was a few seconds here and there when Uditi would zone out.
She’d switch back on again as if nothing had happened, and her mother, Sonam, wasn’t sure if she should worry. Sonam was watching as Uditi dropped a camera on the floor and was confused as to why it was not in her hand. A mother’s hunch hardened: something was wrong.
In early October, a few months after Chakraborty and Ghosh had breakfast with Uditi and her parents, the team received a series of messages from Rajeev on their WhatsApp group. Uditi was taken to the hospital after becoming ill with pneumonia. She was sent home because there was nothing else the doctors could do for her.
The Sarafs looked at what they could find online and tried a number of interventions, such as Indian treatments, a Ketogenic diet and special schools. We were shopping for doctors. We shopped for gods,” says Sonam, but Uditi’s condition slowly worsened.
One of the most important reagents came from abroad. Few researchers use them, and the supply is uncertain. Miranda in Rome was asked by the team to share the antibodies she had developed. She gladly did. She says it was a desperate approach. For me, the priority was to try to help as much as I could.
This condition is called FENIB (familial encephalopathy with neuroserpin inclusion bodies), and the symptoms — which can be similar to dementia — usually manifest late in life. Elena Miranda runs a lab that focuses on the disease at the Sapienza University of Rome. She says that it’s possible that many cases of FENIB go unreported because physicians do not often sequence the genomes of older adults with dementia.
Severe forms of FENIB are very rare. Miranda has known of only three other people with the same mutation that Uditi had. “This form of the disease is very aggressive,” she says.
The disease Uditi was caused by was caused by a single genetic condition that converts a single DNA base from a G to an A. A variation on CRISPR genome editing, called base editing, could theoretically correct exactly this kind of mutation (see ‘Precision gene repair’).
Devinsky also emphasized the difficulties. At that time, base editing — which was first reported in 2016 — had never been tested in a clinical trial. The technique involves shuttling a largeprotein and a smallRNA into affected cells. The brain is one of the most daunting organs and it is difficult to perfect this delivery.
Devinsky assembled a team at NYU Langone Health with expertise in genome editing and neuroscience to conduct preliminary studies of the approach. The researchers pulled together what funding they could from other grants, and the Sarafs funded the rest. “We will sell our house if we have to,” Sonam said.
Jayeeta said that the pressure in the lab was very high. The cells grown in the lab are genetically engineered to be Uditi’s FENIB. A graduate student was asked to repeat the experiment five times after the cells initially didn’t seem to behave as expected. “I was always pushing,” she says. We had to be fast but also be careful. There was not a short cut.
Source: Hope, despair and CRISPR — the race to save one woman’s life
CRISPR, the race to save one woman’s life: a novel treatment for the COVID-19 sickle-cell disease that saves a woman in India
In December 2019, the Sarafs moved back to India. Maintaining a home in the United States was expensive, and Uditi missed her extended family. In January 2021, Uditi was hospitalized with severe COVID-19, when the COVID-19 pandemic struck. Sonam says she spent 20 days in the hospital and was never the same. Communication became increasingly difficult for Uditi and she began to pace the house incessantly, rarely even going to sleep.
Meanwhile, Devinsky had petitioned a US foundation to devise a different experimental treatment called antisense therapy for Uditi. The family flew from India to the United States twice for injections into her spine. The trips became traumatic as her ability to understand the world around her declined.
About an hour and a half away from their home, Debojyoti Chakraborty, a geneticist at the Council of Scientific and Industrial Research’s Institute of Genomics and Integrative Biology in New Delhi, had been making headlines for his efforts to devise a CRISPR-based treatment for a genetic blood disorder called sickle-cell disease.
In India, where there is one of the highest rates of the condition in the world, most people who have it live in impoverished communities. A therapy that could be produced at a fraction of the price charged in the United States is what the group of people hoped to develop.
Source: Hope, despair and CRISPR — the race to save one woman’s life
Avni Genomics in India: a campaign for the cure of duchenne muscular dystrophy and the race to save one woman’s life
Still, that was not the end of their challenges. The genes needed for base editing are longer in the AAV genomes and so they can only carry an additional 4,700 bases. Ghosh and his students worked to divide up their genomic cargo so that it could fit in two separate viruses, and added sequences that would allow the two pieces to be spliced together again when they are expressed inside a cell. The team would inject both viruses in the same place.
It was not the first time Ghosh was swayed by a personal appeal: a few years before he met Uditi, Ghosh came to work and found two women waiting outside of his office. Women said they would not leave until he committed to finding a cure for a genetic condition called Duchenne muscular dystrophy that can be fatal. The women pledged to help raise funds, and Ghosh found himself unable to say no. He has worked on the project and grown close to the families since then.
India has earned a reputation for making complex drugs on a budget. During the COVID-19 Pandemic, Indian manufacturers produced millions of vaccines. Now, the country is manufacturing a malaria vaccine at a fraction of the cost of that in Europe, and it is developing sophisticated cell and gene therapies used in cancer treatments for much less than the price of those in the United States.
Source: Hope, despair and CRISPR — the race to save one woman’s life
Uditi’s Neuronal Stem Cells: A Study of the Impact of AAV Strain on Neuroangiogenesis
Chakraborty took the lead on Uditi’s project. “He is a go-getter kind of person,” says Riya Rauthan, who was then a PhD student in Chakraborty’s lab. He does it regardless of who he wants to ask to get something done.
To minimize interruptions, the team mapped out all of the experiments and the components they would need from start to finish. Projects can be delayed by weeks or months due to lab supply interruptions in India. Everything had to be planned and ordered ahead of time, and Maiti worked to keep the supplies coming, seeking out vendors and negotiating prices. He says that time was more valuable than anything else.
Stem cells were created from Uditi’s blood. She and her colleagues used base editing to reprogram those cells in the lab.
The AAV was prepared to transport the components into Uditi’s neurons. The team needed to determine which strain of AAV would work best — some strains could trigger inflammation in the brain. To find out which type caused less inflammation and how to administer it, the lab tested different types of AAV in mice. The team decided that it was necessary to inject AAV9 into Uditi’s brain.
Some people in the lab took the news hard. Chakraborty thinks that clinicians may become hardened. We do not have that experience. We were not feeling well.
An Indian-origin woman, who underwent a gene-editing treatment after being diagnosed with a rare brain tumour, has said she never thought she’d get sick. Uditi Devinsky, who underwent an experimental treatment, said she couldn’t believe her luck. “When I was born, my father said I wouldn’t be able to live…but…I’m here today,” she added. She was diagnosed with oligodendroglioma, a rare brain tumour.